Psoriasis is a chronic skin condition that affects millions of people worldwide. It is characterized by red, scaly patches on the skin that can cause discomfort and itching. This autoimmune disorder speeds up the skin cell renewal process, leading to excessive buildup on the skin’s surface. While psoriasis is not contagious, it can have a significant impact on a person’s physical and emotional well-being. Understanding its causes, symptoms, and treatment options is essential for managing the condition effectively.
What Is Psoriasis?
Psoriasis is a long-term inflammatory skin disease that occurs when the immune system mistakenly attacks healthy skin cells. This leads to an accelerated production of new skin cells, which pile up and form thick, scaly patches known as plaques. The severity of psoriasis varies from person to person, with some experiencing mild cases and others suffering from severe outbreaks that cover large areas of the body. It can occur in cycles, with flare-ups followed by periods of remission. Some individuals may only experience occasional flare-ups, while others deal with persistent symptoms year-round.
This condition is non-contagious but tends to run in families, suggesting a genetic component. Psoriasis can develop at any age, but it is most commonly diagnosed between the ages of 15 and 35. While it primarily affects the skin, some forms of psoriasis can impact joints and nails, leading to additional complications.
What Causes Psoriasis?
The exact cause of psoriasis is not fully understood, but researchers believe it results from a combination of genetic and environmental factors. The primary cause is an overactive immune system that triggers excessive skin cell production. Here are some key factors that contribute to psoriasis:
Immune System Dysfunction
Psoriasis is an autoimmune disorder, meaning the immune system mistakenly attacks healthy skin cells. This leads to rapid skin cell turnover and the characteristic plaques of psoriasis. The immune response also causes inflammation, which can contribute to itching, redness, and swelling. Scientists believe that T-cells, a type of white blood cell, play a crucial role in triggering this abnormal immune response.
Genetics
Studies show that psoriasis tends to run in families. If one or both parents have psoriasis, their children are at a higher risk of developing the condition. Researchers have identified several genes associated with psoriasis, though having these genes does not guarantee that a person will develop the disease. Environmental triggers often play a role in whether or not genetic predisposition leads to psoriasis.
Environmental Triggers
Certain external factors can trigger or worsen psoriasis symptoms, including:
- Stress: High stress levels can lead to flare-ups. Chronic stress can also weaken the immune system, making it more likely for symptoms to worsen over time.
- Infections: Bacterial and viral infections can stimulate the immune system and trigger psoriasis. Strep throat, for example, is a known trigger for guttate psoriasis in some individuals.
- Weather: Cold, dry climates can worsen symptoms, while humid weather may provide relief. The lack of moisture in cold weather can cause excessive dryness, leading to increased scaling and itching.
- Skin Injuries: Cuts, burns, insect bites, or sunburn can trigger the development of new plaques (known as the Koebner phenomenon). Even minor skin irritations, such as scratches or tattoos, can lead to new lesions in affected individuals.
- Medications: Certain medications like beta-blockers, lithium, and anti-malarial drugs can trigger or exacerbate psoriasis. It is essential for patients with psoriasis to consult their doctor before starting any new medication.
Symptoms of Psoriasis
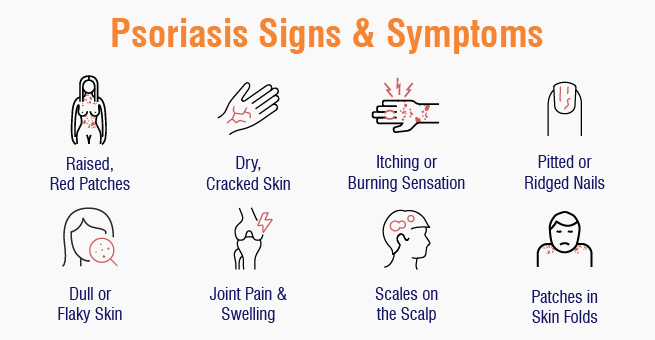
Psoriasis symptoms vary depending on the type and severity of the condition. Common symptoms include:
- Red Patches of Skin – Covered with thick, silvery-white scales, these patches are typically found on the elbows, knees, scalp, and lower back. The patches may vary in size and shape, sometimes merging to cover larger areas of the body. These lesions can be itchy, painful, and prone to cracking or bleeding in severe cases.
- Itching and Burning Sensation – Many people experience discomfort, itching, and a burning or stinging sensation. Scratching the affected areas can worsen inflammation and increase the risk of infection. In some cases, the itching can be severe enough to disrupt sleep and daily activities.
- Dry, Cracked Skin – Affected areas may become extremely dry and prone to cracking and bleeding. Keeping the skin well-moisturized can help reduce the risk of painful cracks and fissures. Cracked skin can also increase susceptibility to bacterial and fungal infections.
- Thickened Nails – Psoriasis can affect fingernails and toenails, leading to discoloration, pitting, or separation from the nail bed. Nail psoriasis can make the nails brittle and cause them to crumble or lift. This can be both cosmetically concerning and functionally impairing.
- Joint Pain – In some cases, psoriasis is associated with psoriatic arthritis, causing stiffness, swelling, and pain in the joints. If left untreated, psoriatic arthritis can lead to permanent joint damage and reduced mobility. Early diagnosis and treatment can help prevent further complications.
Types of Psoriasis
There are several types of psoriasis, each with unique characteristics:
- Plaque Psoriasis (Psoriasis Vulgaris)
- The most common type, accounting for about 80% of cases.
- Characterized by raised, red patches covered with silvery-white scales.
- These plaques can be painful and may crack or bleed, especially in areas subject to frequent movement or friction.
- Guttate Psoriasis
- Appears as small, red spots on the skin, usually triggered by infections like strep throat.
- More common in children and young adults.
- Unlike plaque psoriasis, guttate lesions are smaller and not as thick but can spread rapidly.
Psoriasis Treatment Options
Although there is no cure for psoriasis, various treatments can help manage symptoms and improve quality of life. Treatment options include:
1. Topical Treatments
- Corticosteroids – Reduce inflammation and relieve itching. These are often the first line of treatment for mild to moderate psoriasis.
- Vitamin D Analogues – Help slow down skin cell growth. These can be used alone or in combination with other treatments for better results.
2. Phototherapy (Light Therapy)
UVB Therapy – Controlled exposure to ultraviolet B (UVB) light helps slow skin cell growth. This method is effective for moderate to severe psoriasis and is often used when topical treatments fail.
3. Systemic Medications
Biologic Drugs – Target specific parts of the immune system (e.g., TNF inhibitors, IL-17 inhibitors, IL-23 inhibitors). These are recommended for individuals with severe or treatment-resistant psoriasis.
Conclusion
Psoriasis is a chronic autoimmune condition that requires lifelong management. While there is no permanent cure, advances in treatment options have made it possible for individuals to control symptoms and improve their quality of life. By understanding the causes, symptoms, and available treatments, people with psoriasis can take proactive steps to minimize flare-ups and maintain healthy skin. If you suspect you have psoriasis, consulting a dermatologist is the best way to receive a proper diagnosis and treatment plan tailored to your needs.
