Psoriatic arthritis (PsA) is a chronic autoimmune disease that affects the joints and skin. It occurs in people with psoriasis, a skin condition that causes red, scaly patches. However, psoriatic arthritis is more than just a skin disorder—it leads to joint inflammation, stiffness, pain, and long-term joint damage if left untreated.
Since psoriatic arthritis shares symptoms with other types of arthritis, including rheumatoid arthritis (RA) and osteoarthritis (OA), an accurate diagnosis is crucial. Early detection can help prevent irreversible joint damage and improve a patient’s quality of life. But how exactly is psoriatic arthritis diagnosed?
This guide explores the key steps in diagnosing psoriatic arthritis, including clinical evaluation, blood tests, imaging studies (X-rays, MRI, ultrasound), and other essential diagnostic criteria.
1. Understanding the Symptoms of Psoriatic Arthritis
Before diagnosis, doctors assess signs and symptoms that indicate the presence of psoriatic arthritis. The most common symptoms include:
Joint-related Symptoms:
- Joint pain and stiffness – Often worse in the morning or after inactivity.
- Swelling in fingers and toes – “Sausage-like” swelling (dactylitis).
- Lower back pain – Indicative of spondylitis (inflammation of the spine).
- Enthesitis – Pain where tendons and ligaments attach to bones, such as the Achilles tendon.
- Asymmetrical joint involvement – Unlike rheumatoid arthritis, which usually affects joints symmetrically, psoriatic arthritis can affect different joints on each side of the body.
Skin and Nail Symptoms:
- Psoriasis plaques – Red, scaly patches, often on the elbows, knees, and scalp.
- Nail changes – Pitting, thickening, ridges, or separation from the nail bed.
Other Systemic Symptoms:
- Fatigue – A common symptom due to immune system activity.
- Eye inflammation – Uveitis or conjunctivitis (red, painful, inflamed eyes).
- Digestive issues – Some people with PsA may develop inflammatory bowel disease (IBD).
If a person has psoriasis and joint symptoms, they should consult a rheumatologist for further evaluation.
2. Clinical Examination by a Doctor
The first step in psoriatic arthritis diagnosis is a physical examination performed by a rheumatologist or dermatologist. The doctor will:
- Check for joint pain, swelling, and tenderness.
- Examine the skin for psoriasis plaques.
- Look for nail changes (pitting, ridges, or discoloration).
- Assess mobility and stiffness in affected joints.
- Check for signs of enthesitis and dactylitis.
Since psoriatic arthritis can affect different joints in unique patterns, a detailed clinical evaluation is necessary before moving on to laboratory tests and imaging studies.
3. Blood Tests for Psoriatic Arthritis Diagnosis
While no single blood test can confirm psoriatic arthritis, doctors use several laboratory tests to rule out other conditions, especially rheumatoid arthritis, lupus, and gout.
Common Blood Tests for Psoriatic Arthritis:
A. Rheumatoid Factor (RF) and Anti-CCP Antibody Test
- Used to distinguish psoriatic arthritis from rheumatoid arthritis (RA).
- PsA patients typically test negative for RF and anti-CCP antibodies, while RA patients often test positive.
B. C-Reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR)
- Measures inflammation levels in the body.
- Elevated CRP or ESR suggests active inflammation.
- Not specific to PsA but helps assess disease severity.
C. HLA-B27 Genetic Marker Test
- Identifies the HLA-B27 gene, which is linked to certain inflammatory arthritis types, including psoriatic arthritis with spinal involvement (axial PsA).
D. Uric Acid Test
- Rules out gout, which can mimic PsA symptoms.
While blood tests alone cannot confirm psoriatic arthritis, they help narrow down the diagnosis by eliminating other possibilities.
4. Imaging Tests: X-rays, MRI, and Ultrasound
Imaging studies provide visual confirmation of psoriatic arthritis by detecting joint damage, inflammation, and other structural changes.
A. X-rays
- Show joint damage such as bone erosion and deformities.
- Can reveal pencil-in-cup deformity, a characteristic PsA feature where bone erosion gives joints a tapered appearance.
- Useful for detecting long-term damage.
B. MRI (Magnetic Resonance Imaging)
- Detects early joint and soft tissue inflammation before it appears on X-rays.
- Used to assess spinal and sacroiliac joint involvement.
- More sensitive in detecting enthesitis (inflammation where tendons attach to bones).
C. Ultrasound
- Helps visualize synovitis (joint lining inflammation) and tendon inflammation.
- Can detect early joint changes that may not appear on X-rays.
- Often used in monitoring disease progression.
These imaging techniques help doctors confirm the extent of joint involvement and whether psoriatic arthritis has caused bone or cartilage damage.
5. Psoriatic Arthritis Diagnosis Criteria (CASPAR)
Doctors often use the CASPAR (Classification Criteria for Psoriatic Arthritis) to diagnose PsA. A patient must meet at least three of the following criteria:
- Psoriasis (current, past, or family history)
- Nail changes (pitting, ridges, or separation from the nail bed)
- Dactylitis (sausage-like swelling of fingers or toes)
- Negative rheumatoid factor (RF test)
- Joint changes on X-rays (e.g., new bone formation near joints)
This standardized approach helps doctors differentiate psoriatic arthritis from other types of arthritis.
6. Differential Diagnosis: Ruling Out Other Conditions
Since psoriatic arthritis mimics several other diseases, doctors must rule out:
- Rheumatoid arthritis (RA) – Symmetrical joint involvement, positive RF/anti-CCP.
- Osteoarthritis (OA) – Wear-and-tear arthritis without significant inflammation.
- Gout – High uric acid levels, sudden painful flare-ups.
- Ankylosing spondylitis (AS) – Involves the spine, linked to HLA-B27.
- Lupus (SLE) – Multi-organ involvement, positive ANA test.
A combination of clinical signs, blood tests, and imaging studies is necessary to confirm psoriatic arthritis while excluding other conditions.
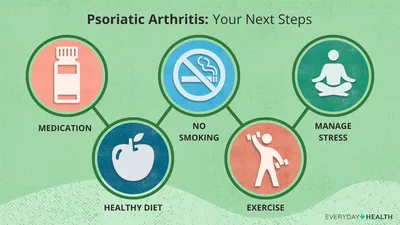
7. Next Steps After Diagnosis: Treatment and Management
Once psoriatic arthritis is diagnosed, the focus shifts to treatment and disease management. A personalized treatment plan may include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) for pain relief.
- Disease-modifying antirheumatic drugs (DMARDs) to slow disease progression.
- Biologic therapies (TNF inhibitors, IL-17 inhibitors, IL-12/23 inhibitors) to target inflammation.
- Physical therapy to improve joint mobility.
- Lifestyle changes, including an anti-inflammatory diet and regular exercise.
Early diagnosis and treatment can prevent severe joint damage, disability, and complications.
Conclusion
Diagnosing psoriatic arthritis requires a comprehensive approach that includes clinical evaluation, blood tests, imaging studies, and exclusion of other conditions. Since PsA shares symptoms with several other forms of arthritis, accurate diagnosis is crucial for timely treatment and better outcomes.
If you suspect you have psoriatic arthritis, consult a rheumatologist for an early diagnosis and personalized treatment plan. Early intervention can help preserve joint function, reduce pain, and improve overall quality of life.
